Presently there is a significant unmet clinical need whereby metastatic bone disease (MBD) most commonly occurs in spinal vertebrae and is linked to a substantial deterioration in patient quality of life through bone pain, fracture and spinal cord injury (SCI). In the UK:
As such these terminally-ill patients are recognised as having unique and personalised care needs.
MBD in the spine destroys the bone in the vertebrae
Thus weakening it and increasing the risk of fracture. This may lead to spinal cord injury with permanent paralysis and significant additional pain.
The prognosis for patients with MBD is poor, with life expectancy usually less than 18 months. Medical costs associated with MBD are significantly higher (€50K/annum) than those of MBD-free cancer patients.
Current care options include:
- conservative treatments (analgesics),
- radiotherapy (reduces pain but not instability, and increases fracture risk),
- major surgery (recuperation time of 2 -6 months versus life expectancy of less than 18 months and risks the spread of the tumour cells) or percutaneous vertebroplasty (PVP) where PMMA cement is injected into the fractured vertebrae.
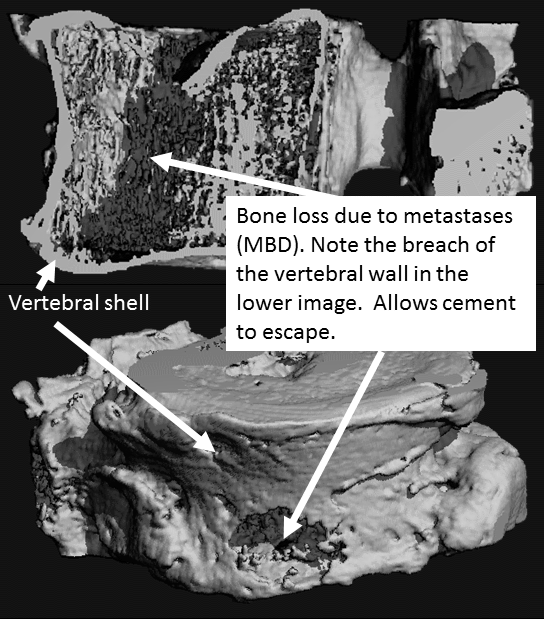
Percutaneous vertebroplasty (PVP) has been used, post-fracture, in osteoporosis, but PVP suffers from severe complications that considerably reduce its effectiveness in spinal MBD and are as follows:
- PVP uses low injection cement-volumes that provide pain relief but offer no mechanical support, which is necessary to prevent catastrophic vertebrae failure.
- Previous work by Prof Richard Hall notes that cement flows are idiosyncratic and depend on e.g. formulation and bone morphology. Hence it is difficult to place cement where structural support is needed, thus lesion/patient specific needs cannot be satisfied.
- In MBD, the vertebra shell is often compromised (Figure above) leading to cement leakage near the spinal cord or aorta (PMMA is highly exothermic).
“This funding will enable us to significantly expand our work combining computational modelling with cutting-edge imaging to better understand how cancers grow and interact with surrounding tissues.
We are excited to use these multidisciplinary frameworks to understand vertebra fracture risk and ultimately help to improve quality of life for cancer patients.”

Research and Innovation Lead and Co-investigator of the OncoEng collaboration at UCL
The NHS Long Term Plan for Cancer, The EU Breast Cancer Roadmap (2017) and the Global Status of Metastatic Breast Cancer (2016) call for new interventions that improve quality of life, identify bone fractures & reduce spinal cord injury. It is extremely challenging for an implant to support the MBD degraded vertebrae. Lesions vary enormously, both morphologically and mechanically, presenting unmet challenges in terms of designing and manufacturing a bespoke implant to conform to the geometric and load/strain environment in which too little support will lead to fracture.
In response to these significant clinical needs OncoEng will develop:
(1) a Prophylactically-Amenable, Lesion-Specific, Minimally-Invasive Implant (MII) to support the verebrae load and prevent fracture, thus significantly inhibiting instability, bone pain and SCI.
(2) an integrated, multiscale, Fracture Prediction Framework to identify those vertebrae at risk of fracture, so as to aid a prophylactic intervention to reduce risk and enable the lesion-specific nature of the MII.
Latest News
Using statistical shape models to develop generalised models of vertebrae
Within OncoEng, the team at UCL aims to develop state-of-the-art imaging and computational tools to predict the growth of metastatic lesions and how these can result in fractures in the spine. This involves a variety…
Metamaterials Explored: Our Experience at the 2023 UK Metamaterials Network Conference
This June, Ryan and I had the privilege of attending the UK Metamaterials Network conference at the scenic Wotton House. Over three insightful days, we delved deep into the diverse world of metamaterials, exploring their…
Exploring Metastatic Bone Disease Through Patient Narratives
As a mechanical engineer looking to develop methodologies to characterise spinal biomechanics and its perturbation due to metastatic bone disease (MBD), attending the OncoEng Patient Day was an eye-opening experience. This event provided an invaluable…
Birmingham Med-Tech Innovation Expo 2023
Blog written by Yash Karade and Aamena Lakdawala We bid farewell to Leeds on the morning of 7th June 2023 as we started our journey to the MedTech Expo in Birmingham. It was surely a…
World Cancer Day
The Leeds Cancer Research Centre will be delivering a mini-conference as part of World Cancer Day on the 3 rd February (World Cancer Day is actually on 4th Feb). OncoEng is very supportive of the…

OncoEng Quarterly Meeting
Great OncoEng Quarterly get together last week. The Management Board Meeting in the morning was eagerly attended by all the researchers and academics. In the afternoon we were joined by Dr Sherron Furtado, Craig Gerrand, Sarah Astill and David Lunn to…